Cystic Acne Is Severe Acne, and Includes Large Lesions (Nodules and/or Cysts) That Are 5 mm or More in Diameter

The Essential Info
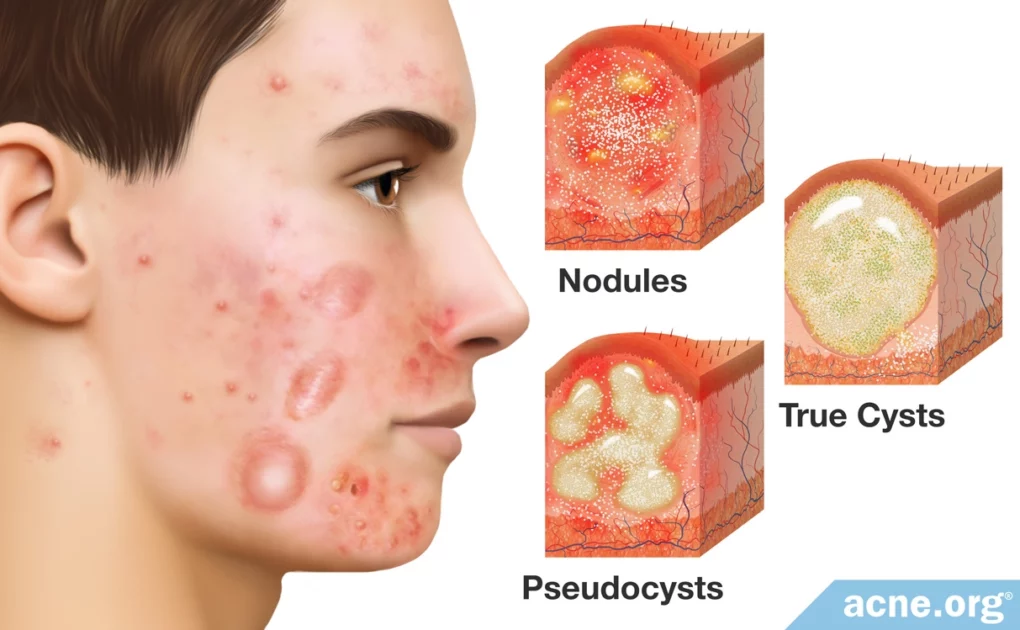
Cystic acne, also called nodulocystic acne, is a severe type of acne consisting of larger, more painful lesions called nodules and cysts.
- Nodules: Nodules are by far the most common nodulocystic acne lesion type. They are large (over 5 mm in diameter), fibrous, raised lesions that feel firm to the touch.
- Cysts: Cysts are much more rare. They are large (usually over 7 mm in diameter), liquid or pus-filled lesions that feel semi-soft and movable.
Treatment
Cystic lesions can take weeks or even months to resolve and are extremely prone to scarring. This is why it is vitally important that people with cystic acne treat their skin early and aggressively to reduce the potential for scarring.
Normally, nodules and cysts can be prevented with a properly-applied benzoyl peroxide regimen.
However, for cases of severe, widespread, and scarring cystic acne, isotretinoin (Accutane®) is normally what dermatologists recommend. Isotretinoin should be the option of last resort since it permanently changes the skin and body and can come with lifelong side effects. It also causes severe birth defects or miscarriage.
For an occasional nodule or cyst, a quick trip to the dermatologist for a cortisone injection directly into the lesion can quickly initiate healing and reduce scarring.

The Science
Cystic acne, also called nodulocystic acne, is a severe form of acne that comes with large (over 5 mm in diameter), red, sore acne lesions called nodules and cysts on the face, neck, back, and chest.
Cystic acne is the same disease as regular acne, just more severe. All acne starts when tiny hair follicles, called pores, become clogged. This clog results in a buildup of skin oil, dead skin cells, and bacteria inside the pore. Ultimately the pore can burst, which leads to the redness and soreness that we see in acne lesions. If the pore bursts especially deep within the skin, this can lead to the severe lesions we see in nodulocystic acne: nodules and cysts.
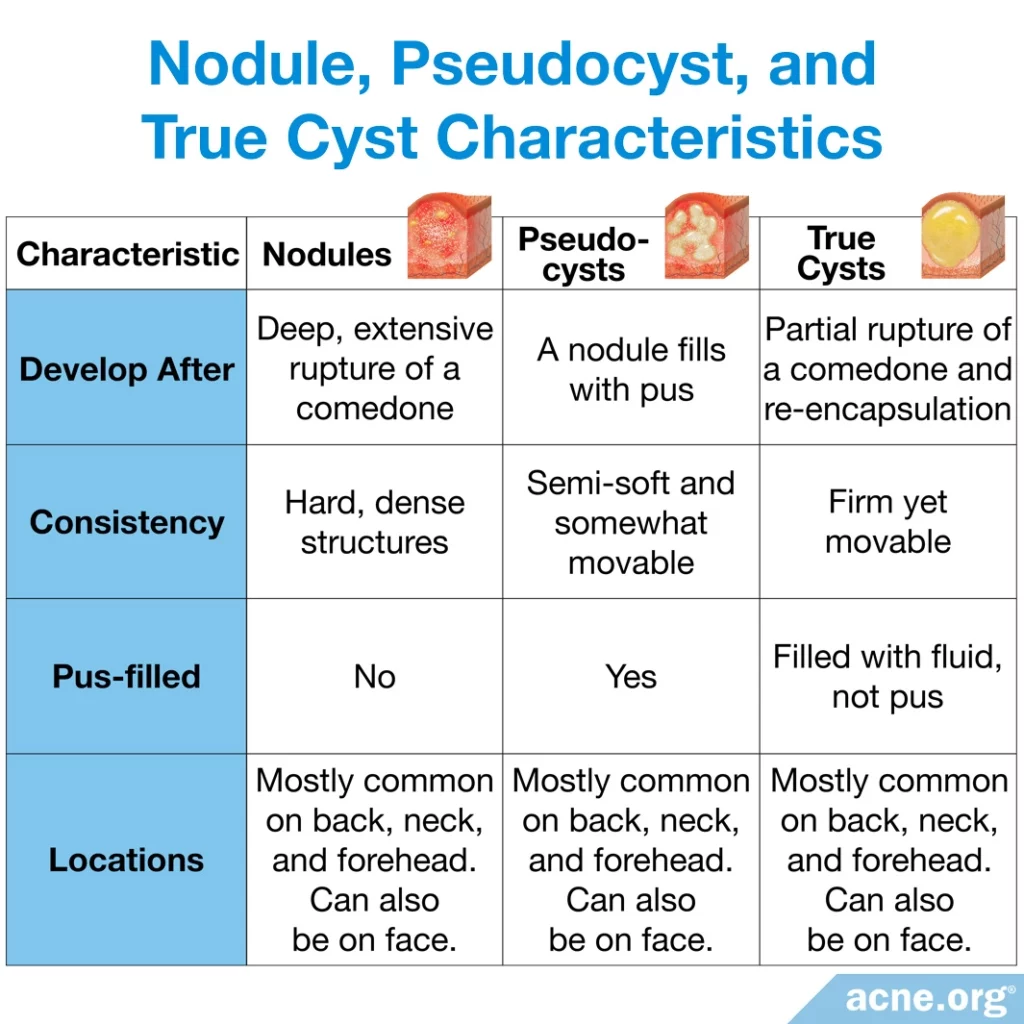
A Closer Look at Acne Nodules and Cysts
Nodules
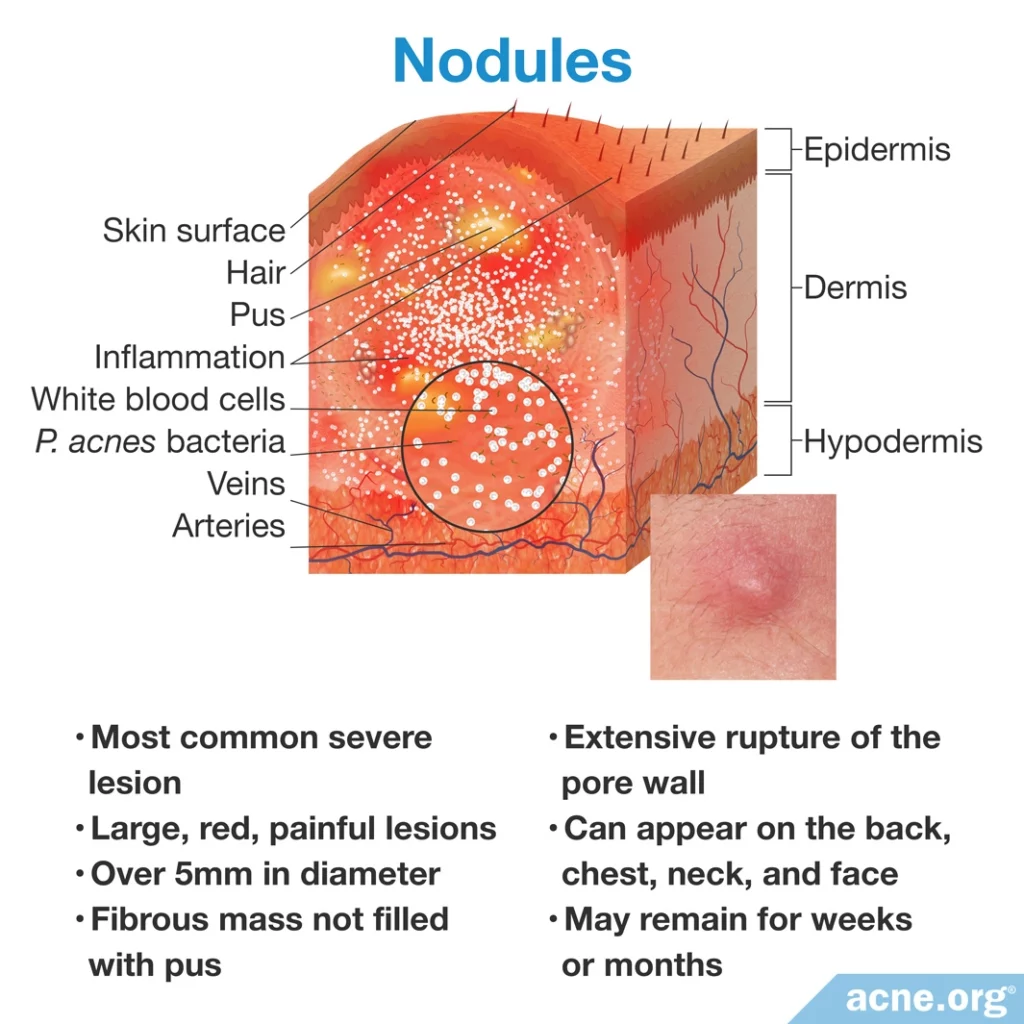
Nodules are much more common than cysts.
They appear as large, red, painful lesions over 5 millimeters in diameter. They are not filled with pus, and instead are solid fibrous masses.
Nodules develop when there is an extensive rupture of the pore especially deep within the skin, which dermatologists often refer to as a “complete explosion of a pore.”
They tend to appear on the back, neck, forehead, and chest. This is likely because these regions have pores with larger skin oil-producing glands.
Due to the extensive damage caused by the pore rupture, nodules may remain for weeks or months before healing.
Cysts come in 2 types:
- Pseudoysts: More common, filled with pus
- True Cysts: Rare, filled with fluid
Pseudocysts
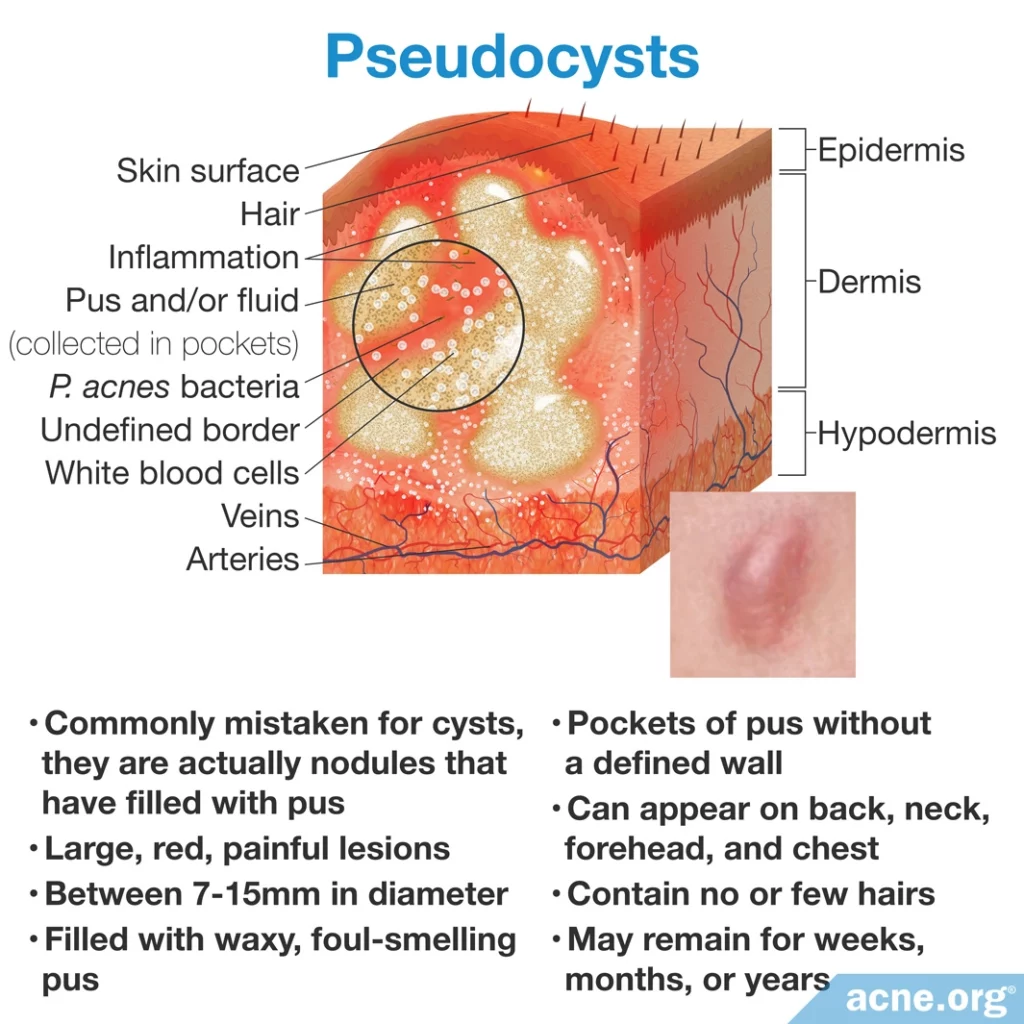
Most acne cysts are best described as pseudocysts because in reality they are simply nodules that fill with waxy, foul-smelling pus. However, for clarity, the dermatology community uses the term “cyst” to refer to pseudocysts.
Similar to nodules, pseudocysts also tend to appear on the back, neck, forehead, and chest.
Pseudocysts can be stubborn, remaining for months or even years before healing.
True Cysts
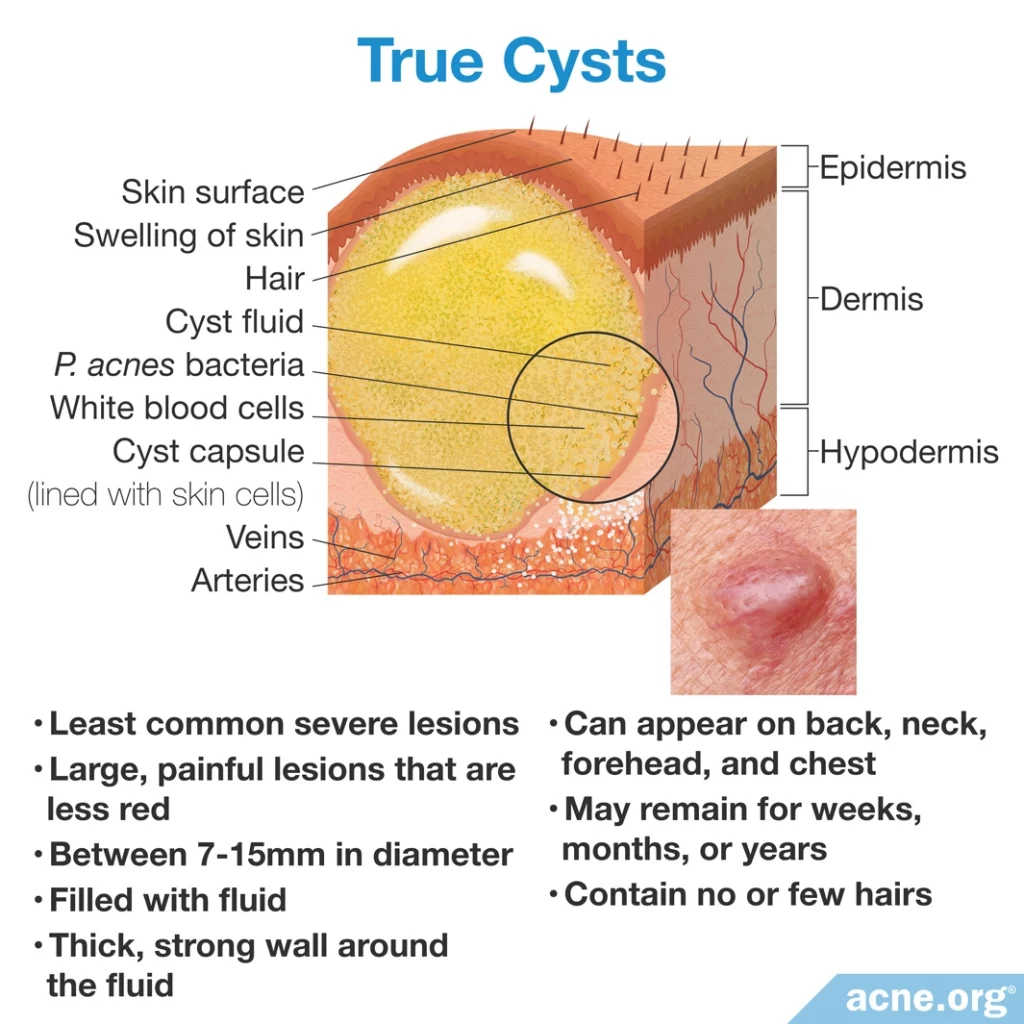
True cysts appear as large, red, painful lesions between 7 – 15 millimeters in diameter.
Unlike nodules, true cysts are filled with fluid that can be felt as it moves beneath the skin when touched.
They develop when only a small area of the pore wall bursts, and instead of releasing its contents into the skin, the body builds a thick and strong secondary wall around the expelled contents.
Similar to nodules and pseudocysts, true cysts also tend to appear on the back, neck, forehead, and chest.
Like pseudocysts, true cysts may remain for months or even years before healing.
The table below displays the characteristics of nodules and cysts:
Causes of Nodulocystic Acne
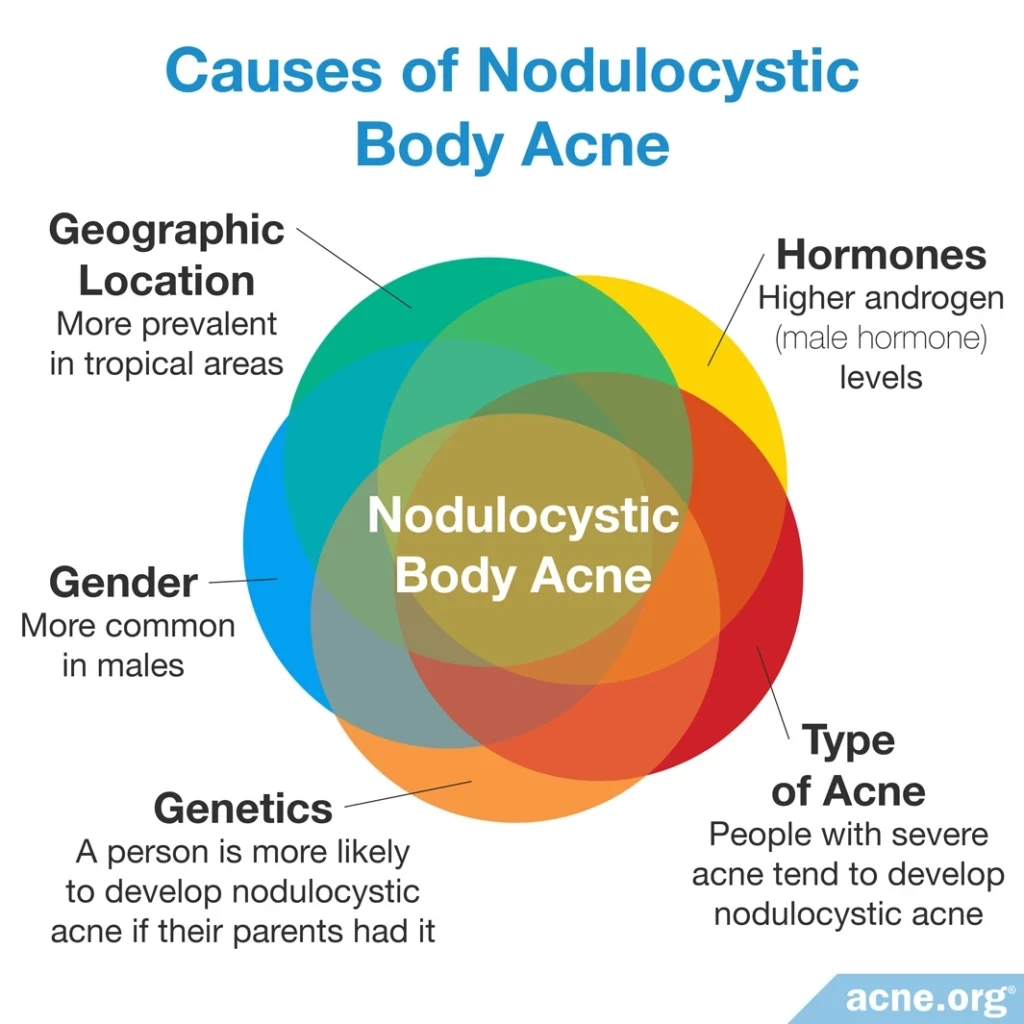
No one knows exactly what leads to nodulocystic acne in one person and not in another, but some common threads may help explain its development.
- Genetics: A person is more likely to develop nodulocystic acne if his/her parents experienced it. As such, there may be a genetic component to some cases.
- Hormones: Androgens, which are male hormones found in both males and females, are highly associated with acne, including nodulocystic acne. Generally speaking, increased androgen levels, including dehydroepiandrosterone sulfate (DHEA-S) and testosterone, result in more severe acne because they increase the production of skin oil (sebum).
- Gender: Especially severe nodulocystic acne is more common in males. However, females can develop this form of acne too, and are at a higher risk of developing it during pregnancy.
- Geographic location: Nodulocystic acne is more prevalent in tropical areas of the world, but the reason for this is unknown.
- Type of acne: People with more acne lesions and more widespread acne tend to develop nodulocystic acne. In comparison, people who have only a few lesions and only facial acne are less likely to develop nodules or cysts.
Treatment of Nodulocystic Acne
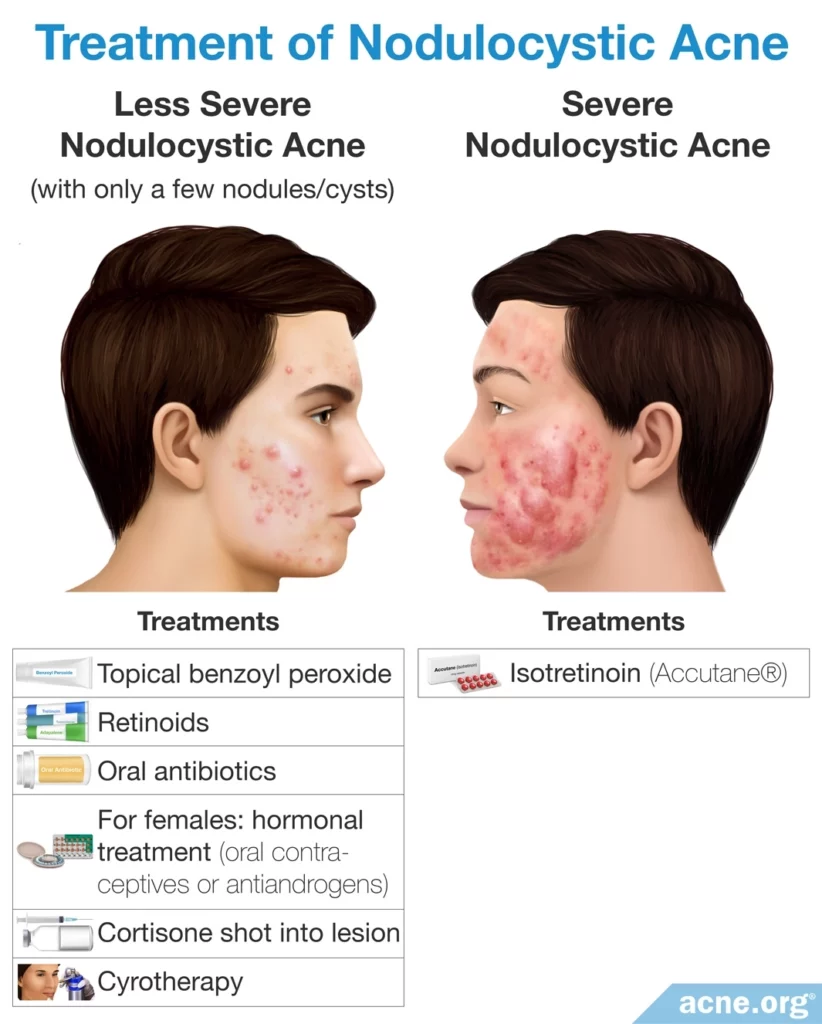
Topical treatments
Less severe cases of nodulocystic acne, with only a few cystic lesions, are often treated with topical benzoyl peroxide or retinoids (tretinoin, adapalene, tazarotene), or a combination of the two.
Oral antibiotics
Doctors sometimes add oral antibiotics to a treatment plan. They may provide some temporary relief, but should only be used for a maximum of 3 months.
Isotretinoin (Accutane®) – for more severe cases
For people with severe nodulocystic acne, doctors may prescribe the oral medication, isotretinoin, often known by its brand name, Accutane®, normally for 15 – 20 weeks. However, isotretinoin causes severe and sometimes lifelong side effects, as well as birth defects, so its use should be carefully considered alongside a trusted physician, and never as a first-line treatment.1-12
Hormonal treatments – females only
Doctors will sometimes prescribe hormonal treatment, such as oral contraceptives or anti-androgen medications, to females with nodulocystic acne.
Cortisone shots – treating one lesion at a time
A shot of cortisone directly into a nodule or cyst can significantly help heal it and prevent scarring. Cortisone shots are effective and helpful, but should only be used on one, or a few, nodules or cysts at one time.
Cryotherapy – treating one lesion at at time
A doctor or nurse can apply extreme cold directly to a lesion to “kill” the lesion.
Oral Dapsone – a potential new option for cases where isotretinoin fails to help?
Severe nodulocystic acne is sometimes unresponsive even to isotretinoin. One case study suggests that oral dapsone might become a promising alternative treatment for nodulocystic acne when isotretinoin fails.13 However, much more research on this potential treatment is necessary.
Cystic Acne Scarring
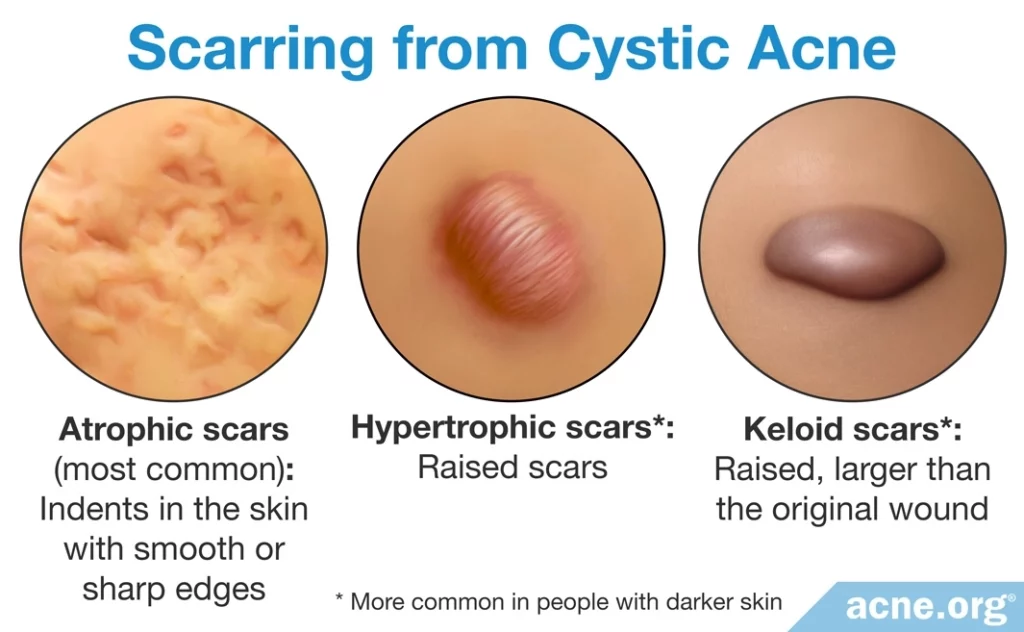
Nodulocystic acne often causes scarring. Normal acne can also scar, but generally causes less severe scars than those from nodules or cysts.
The scarring associated with nodulocystic acne is the reason it is important to treat nodulocystic acne promptly.
There are three main types of acne scars that nodules or cysts can leave behind.
- Indented (most common): Indented scars, called atrophic scars, appear as indents in the skin with smooth or sharp edges. They are the most common type of scars.
- Raised: Raised scars, called hypertrophic scars, appear as elevations above the skin. When they first form, they are the same size as the original cyst or nodule, but over time these elevated scars may decrease in size. Non-Caucasian people are more prone to develop hypertrophic scars.
- Raised (Keloid): Keloid scars are a specific kind of hypertrophic scar that are bigger than the original cyst or nodule, and do not decrease with time. Non-Caucasian people are also more prone to develop keloid scars.
Because cystic acne scars often are large, they can cause significant emotional distress. This emotional suffering can cause people to miss school or work and can even sometimes cause patients to refrain from seeing a doctor. However, the longer cystic acne goes untreated, the worse the scarring can be. Therefore, it is important that patients suffering from cystic acne seek out treatment immediately to prevent severe scarring.14
Rare Forms of Nodulocystic Acne
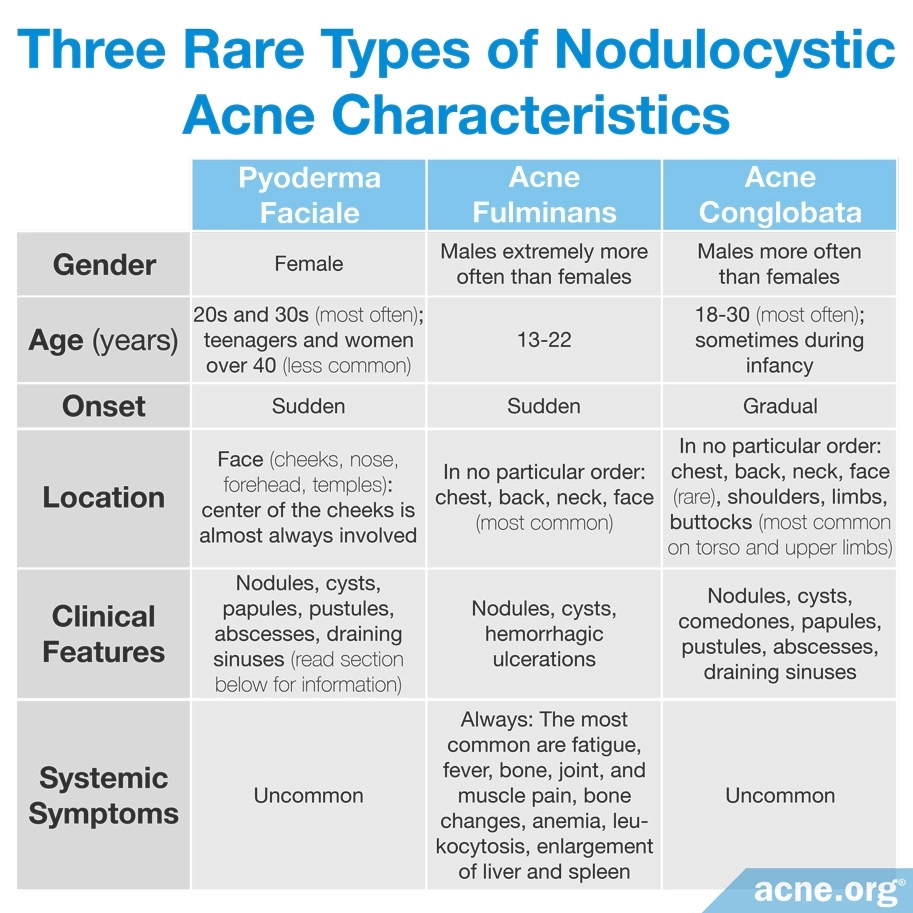
In addition to general nodulocystic acne, there are three rare forms of the nodulocystic variety that are unique.
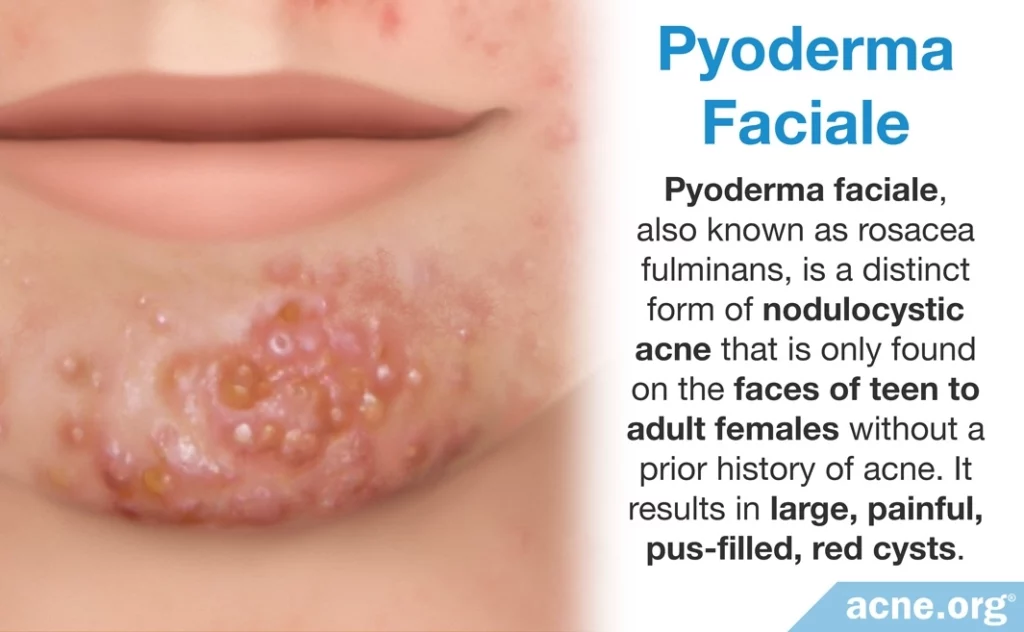
- Pyoderma faciale, also known as rosacea fulminans, is a distinct form of nodulocystic acne that is only found on the faces of females. It results in large, painful, pus-filled, red cysts mainly on the central region of the cheeks. Redness around these lesions can be intense. Generally, pyoderma faciale develops in teen to adult females without a prior history of acne. It is normally treated with a steroid called oral prednisolone at a dosage of 1mg/kg every day for one to two weeks–with gradual reduction of the dose during the following two to three weeks–combined with isotretinoin at a dosage of 0.2 – 0.5mg/kg daily later in the course. Treatment with isotretinoin continues until all lesions are cleared, which can take up to four months.
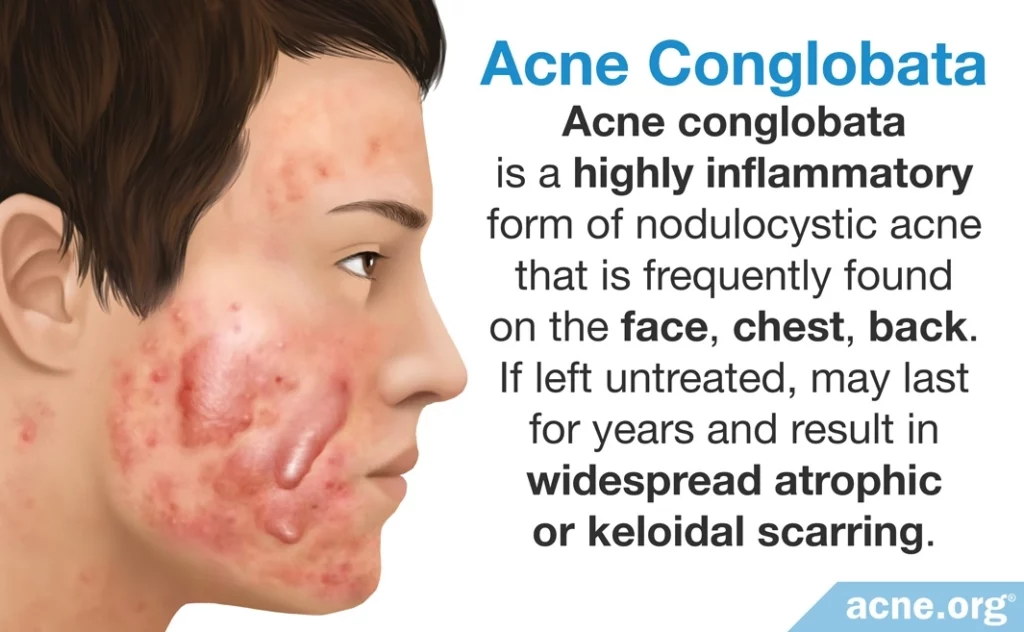
- Acne conglobata is a distinct form of nodulocystic acne that is frequently found on the face, chest, back, and limbs of boys and young males, especially those who live in warmer climates. This acne type is highly inflammatory and presents a mixture of comedones, papules, pustules, nodules, and/or cysts. Acne conglobata, if left untreated, may last for years and result in widespread atrophic or keloidal scarring.
- Acne fulminans is a distinct form of nodulocystic acne that is commonly present on the chest, back, neck, and face. It includes nodules, cysts, and hemorrhagic ulcerations (bleeding ulcers) and is accompanied by other symptoms, including fever, fatigue, pain in the joints and bones, and weight loss. The lesions and symptoms of this type of acne most commonly affect adolescent Caucasian males.11

This table compares the three rare types of nodulocystic acne:
Rarely, a severe form of acne can be part of a more complex syndrome, such as:
- SAPHO syndrome: Besides acne, people with this syndrome suffer from synovitis (joint inflammation), pustulosis (blisters on the hands and/or feet), hyperostosis (excessive bone growth), and osteitis (bone inflammation).
- PASH syndrome: Besides acne, people with this syndrome suffer from pyoderma gangrenosum (painful ulcers on the legs) and hidradenitis suppurativa (lumps in the armpits and groin).15,16
Draining Sinuses
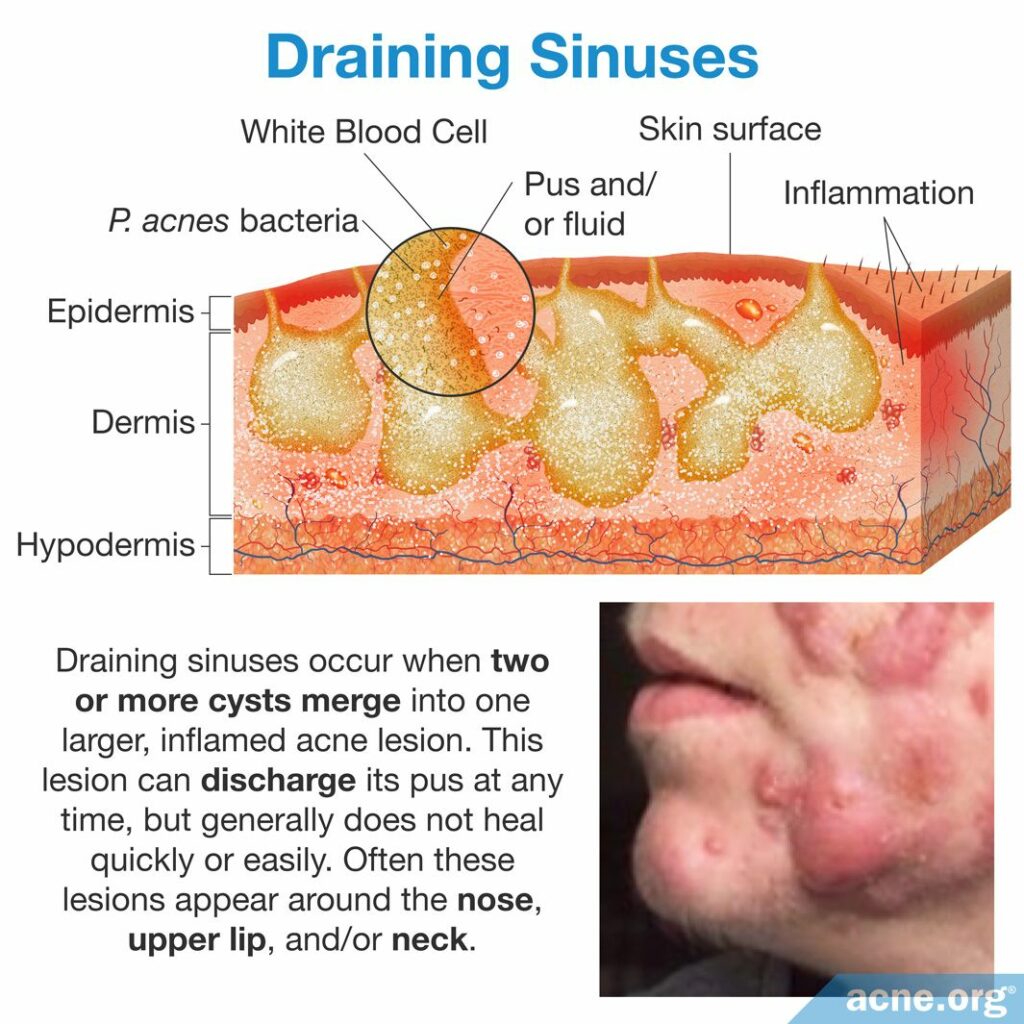
Occasionally, lesions called draining sinuses develop in patients suffering from nodulocystic acne. They are especially common in people who suffer from one of the three rare forms of nodulocystic acne described above. Draining sinuses occur when two or more cysts merge into one huge (several cm long), inflamed acne lesion. This lesion can discharge its pus at any time, but generally does not heal quickly or easily. Often these lesions appear around the nose, upper lip, and/or neck.17
References
- Brogden, R. & Goa, K. Adapalene. Drugs 53, 511 – 519 (1997). https://www.ncbi.nlm.nih.gov/pubmed/9074847
- Gollnick, H. Current concepts of the pathogenesis of acne. Drugs 63, 1579 – 1596 (2003). https://www.ncbi.nlm.nih.gov/pubmed/12887264
- Oberemok, S. & Shalita, A. Acne vulgaris, I: Pathogenesis and diagnosis. Cutis 70, 101 – 105 (2002). https://www.ncbi.nlm.nih.gov/pubmed/12234155
- Toyoda, M. & Morohashi, M. Pathogenesis of acne. Med. Electron Microsc. 34, 29 – 40 (2001). https://www.ncbi.nlm.nih.gov/pubmed/11479771
- Thiboutot, D. The role of follicular hyperkeratinization in acne. J. Dermatol. Treat. 11, 5 – 8 (2000). https://www.tandfonline.com/doi/abs/10.1080/095466300750163645
- Pus https://en.wikipedia.org/wiki/Pus
- Buxton, P. ABC of Dermatology (4th ed). 49 (Blackwell Publishing, 2003). http://famona.sezampro.rs/medifiles/abc/abc of dermatology.pdf
- Orentreich, N. & Durr, N. The natural evolution of comedones into inflammatory papules and pustules. J. Invest. Dermatol. 62, 316 – 320 (1974). https://core.ac.uk/download/pdf/82174419.pdf
- Acne https://en.wikipedia.org/wiki/Acne
- Arndt, K. Manual of Dermatologic Therapeutics (7th Edition). 5 – 8 (LWW (PE), 2007).
- Habif, T. P. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 231 – 233 (2016). https://www.elsevier.com/books/clinical-dermatology/habif/978-0-323-26183-8
- Plewig, G. & Kligman, A. Acne and Rosacea. (Springer International PU, 2000). https://www.springer.com/gp/book/9783642640964
- Al-Kathiri, L. & Al-Najjar, T. Severe nodulocystic acne not responding to isotretinoin therapy successfully treated with oral dapsone. Oman Med. J. 33, 433‐436 (2018). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6131924/
- Layton, A., Henderson, C. & Cunliffe, W. A clinical evaluation of acne scarring and its incidence. Clin. Exp. Dermatol. 19, 303 – 308 (1994). https://www.ncbi.nlm.nih.gov/pubmed/7955470
- Nguyen, M. T., Borchers, A., Selmi, C., Naguwa, S.M., Cheema, G. & Gershwin, M. E. The SAPHO syndrome. Semin. Arthritis Rheum. 42, 254‐265 (2012). https://www.ncbi.nlm.nih.gov/pubmed/23153960
- Ead, J. K., Snyder, R. J., Wise, J., Cuffy, C., Jafary, H. & Fischborn, K. Is PASH syndrome a biofilm disease?: A case series and review of the literature. Wounds 30, 216‐223 (2018). https://www.ncbi.nlm.nih.gov/pubmed/30212364
- Jansen, T., Lindner, A. & Plewig, G. Draining sinus in acne and rosacea. A clinical, histopathologic and experimental study. Hautarzt 46, 417 – 420 (1995). https://www.ncbi.nlm.nih.gov/pubmed/7642386