Last month, Ryan Reynolds’ colon made an appearance on national television. After losing a bet with his Wrexham Association Football Club co-owner Rob McElhenney over learning Welsh, Reynolds agreed to have his experience getting a colonoscopy aired as a PSA on CBS Mornings, in collaboration with the Colorectal Cancer Alliance. McElhenney got one, too. On both of their colonoscopies, their doctors snared away polyps, or abnormal growths of tissue inside of their colons with the potential to turn into cancer one day. When Reynolds and McElhenney both woke up from their anesthesia, their physicians (and the headlines that soon followed) applauded them for undertaking a potentially lifesaving procedure.
The results of a recent large European trial looking into colonoscopies, however, has called that statement into question for some (Bloomberg’s headline, for example: “Screening Procedure Fails to Prevent Colon Cancer Deaths in Large Study”). As a resident physician who frequently discusses colon cancer screening with my patients, I want to be clear: If you’re planning to have a colonoscopy soon, you shouldn’t cancel your test. But going forward, in light of this study, it may be worth reconsidering how we use them for colon cancer screening—and even reconsidering whether they should be characterized as a necessary rite of passage.
Published this month in the prestigious New England Journal of Medicine, the NordICC Study Group trial investigated the effectiveness of colonoscopies as a population-level screening tool for colorectal cancer. Including more than 84,000 middle-age individuals in Norway, Poland, and Sweden, the trial compared the likelihood of getting colon cancer, dying from colon cancer, and dying from any cause over 10 years among people who were and were not invited to get a colonoscopy. It was a randomized-control trial, the gold standard for evidence in medicine, and the first time that this kind of trial had been done for the colonoscopy. The results were highly anticipated, and ultimately surprising. For the group invited to get a colonoscopy, the investigators found a modest decrease in the incidence of getting a colon cancer diagnosis (about 18 percent) but no change in the likelihood of dying from either colon cancer or any other cause during the study period. In other words, there is a benefit to doing colonoscopies for cancer screening, but it’s smaller than what we’ve generally expected. A research highlight in Nature called the results “disappointing.” After all, the hope of performing cancer-screening colonoscopies—an invasive and resource-intensive test—is to help people not die.
Now, there are lots of caveats to the study, and again, if you have a colonoscopy coming up, you shouldn’t cancel it. Most importantly, the NordICC study was a pragmatic one, designed to mimic clinical practice in real life. The team’s intervention was inviting individuals to get a colonoscopy; it wasn’t the procedure itself. Only 42 percent of patients took doctors up on their offer for a colonoscopy. Among those who actually did get the procedure, the likelihood of either getting or dying from colon cancer decreased significantly over the 10-year period relative to those who didn’t. In the United States, where screening colonoscopies are far more common, the estimated uptake for some groups is closer to 70 percent at best. But many people may still be on the fence about getting an invasive procedure that requires days of prep, changes to your diet, and taking time off work.
Then, there are a few other things to note about the study’s design. From prior studies, we know Black individuals are at higher risk for colon cancer, but we don’t know how well represented they were in this study from what has been published. As others have pointed out, the study period of 10 years may not have been a long-enough time to see a meaningful difference in outcomes. Doctors have also gotten much better at finding polyps on colonoscopies since the trial started in 2009. And perhaps most importantly, the study was done on the general population, so it doesn’t apply for high-risk people who have a family history of early colon cancer or have conditions like ulcerative colitis or Crohn’s disease. The primary question the trial answered is an important one for governments that fund colon cancer screening programs, and for doctors thinking about what to recommend to their patients, but not really for individuals getting one.
Nevertheless, the NordICC study overall was well designed, and it should raise questions about how best to screen for colon cancer as a society. The United States largely stands alone in recommending colonoscopy as a first-line screening test. Because of the colonoscopy’s spot in the limelight in the U.S., you might be surprised to learn that there even are other options. Most industrialized countries with robust screening programs for colon cancer favor other means of detection. Some, like the United Kingdom, recommend stool-based tests first, like fecal occult blood testing or fecal immunochemical testing—also designated as FIT—to screen for fragments of blood in your stool, followed by a colonoscopy to further investigate any abnormal findings. Others, like Italy, recommend sigmoidoscopy. This is similar to a colonoscopy, but it only examines the lower third of the colon (known as the left side), checking where most polyps tend to be found, and requires less cleanout of the bowel before the procedure, with an enema and fewer laxatives.
These recommendations in other countries are based on older data from randomized-control trials, showing benefit in reducing the likelihood of dying from colon cancer for stool-based tests and sigmoidoscopy, both of which can be easier for patients. The U.S. guidelines today, taking into account prior observational studies and expert opinion, put first-line colonoscopy on an equal playing field with those other options. Yet despite this parity on paper, colonoscopies in reality are often held up among many patient advocacy groups and doctors as the gold standard for screening.
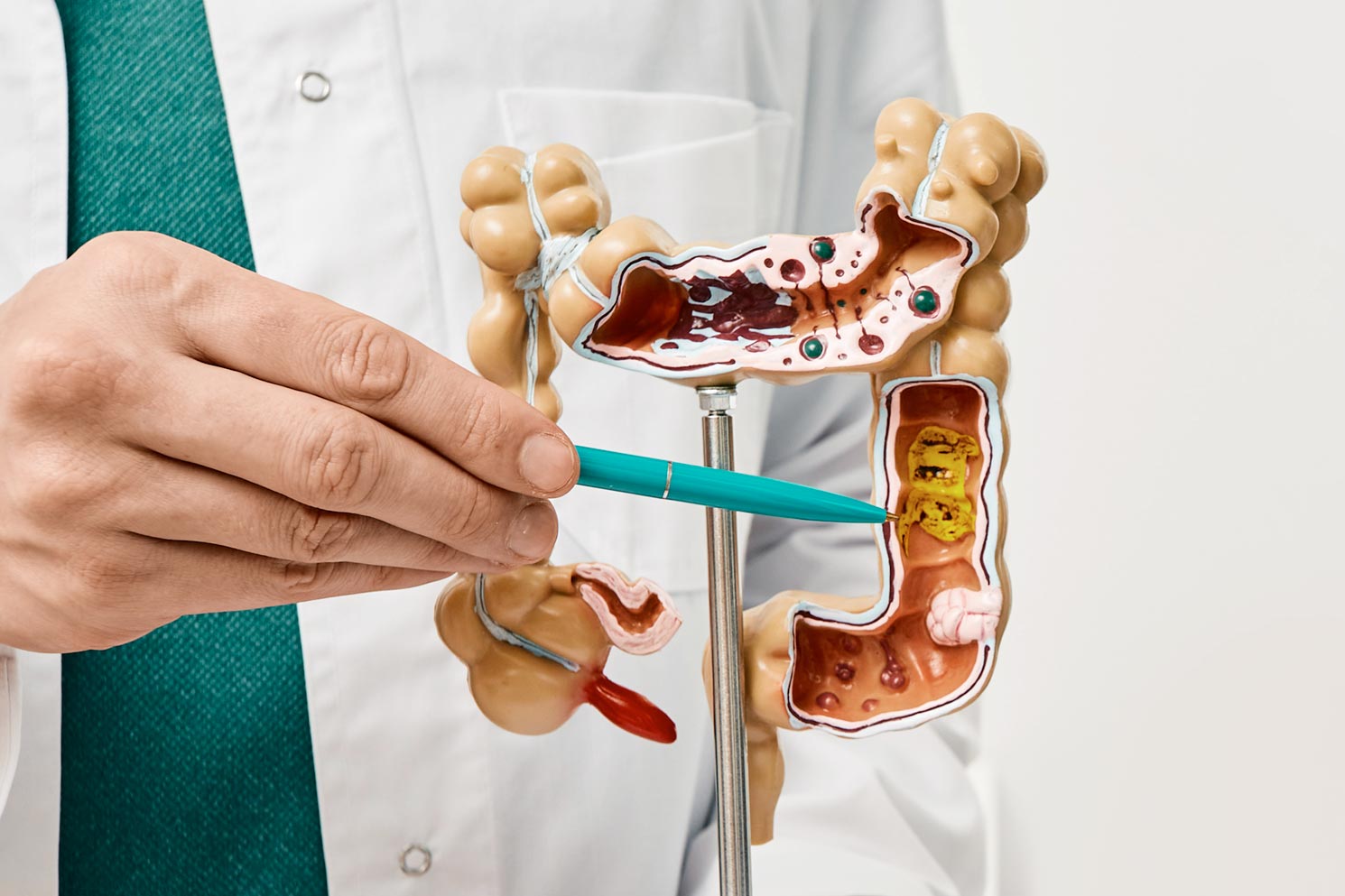
The American attachment to screening colonoscopy perhaps explains why the NordICC team’s results have been so jarring here in the United States and feel, in some ways, like a betrayal. Over the past week, gastroenterology-oriented medical societies and key physician voices have come out in full force, blasting outlets like CNN for sensationalist coverage of the study and taking to Twitter to strongly reiterate that colonoscopies save lives. And for good reason: The colonoscopy floats on rarefied air as the perfect cancer screening test in theory. Unlike a stool test for colon cancer—or, for that matter, mammography for breast cancer or a chest CT scan for lung cancer—a colonoscopy allows for doctors to both diagnose and snare away polyps right then and there before they could morph into cancer a decade or two later. And unlike a sigmoidoscopy, a colonoscopy also examines the right side of the colon, where polyps could hide and turn into cancer, too. (Reynolds’ polyp, for example, was lurking further into his colon.)
Cynics have pointed to how lucrative colonoscopies are to explain the outrage. I think the staunch colonoscopy defenders are being a bit subjective, but for a different reason. Recommending a screening colonoscopy intuitively feels like practicing good medicine. Colon cancer is highly visible in American life. Today, it is among the most common cancers affecting Americans, and it’s increasingly reaching younger people for reasons that remain unknown. It has claimed the lives of high-profile celebrities such as Chadwick Boseman. In that context, the colonoscopy has become more than just a routine cancer screening test. It has turned into a rite of passage introducing middle age, complete with a set of rituals that include consuming a clear liquid diet, voluntarily inducing diarrhea by drinking copious oral laxatives, and spending a morning or afternoon simmering in an anesthetic-powered haze of bliss. Vigorous, well-intentioned public advocacy, complete with PSAs starring A-list celebrities—Will Smith and Katie Couric have also made entries in the colonoscopy-recording genre—only further cemented the colonoscopy’s position as both a cultural touchstone and the go-to way to screen for colon cancer.
Reducing the incidence of colon cancer, through a superbly safe test, is a noble goal. And we shouldn’t get rid of the colonoscopy as a screening method. The NordICC team’s findings suggest, however, that maybe we’ve oversold the benefits of screening colonoscopies—as the study’s lead author, Michael Bretthauer, pointed out to Stat earlier this month—while implicitly underselling tests like FIT that are also backed by good data.
Right now, major studies are in progress comparing methods of colon cancer screening head to head. But for now, in the wake of the NordICC study’s results, perhaps we should try to peel back the cultural influence of the colonoscopy, both in the exam room and in our public health messaging. The best screening test, ultimately, is the one that a person is most likely to actually go out and complete. We also know that colon cancer screening rates in the U.S. still have a lot of room to grow. Among average-risk people, some might prefer the once-in-a-decade screening ability that a colonoscopy offers; others who can’t take a weekday off work easily, or face transportation barriers to and from their procedure, might opt for an annual FIT test instead, which just involves a trip to the bathroom. Maybe, in their next PSA for colon cancer screening, McElhenney can get a colonoscopy while Reynolds documents his experience taking a FIT test. It may not make for the best television, but it could maybe save even more lives and meet more people where they are.